Study Reveals Need for Updated Iron Deficiency Guidelines in Pregnancy

A study aimed to extend a physiologically based method for determining serum ferritin (SF) concentration thresholds for iron deficiency (ID) in healthy pregnant women. Previous research has shown that in nonpregnant women, a decline in hemoglobin (Hb) and a rise in soluble transferrin receptor (sTfR1) concentrations can be used to identify the onset of ID.
Heavy Menstrual Bleeding: Key Cause of Iron Deficiency

Heavy menstrual bleeding is the most common cause of iron deficiency (ID) and iron deficiency anemia (IDA) in reproductive-aged women, significantly affecting their quality of life. These conditions are often normalized by society and healthcare providers, leading to underdiagnosis and inadequate treatment. The adverse impacts of bleeding and ID/IDA include diminished cognitive function, increased work and school absenteeism, and presenteeism. Furthermore, evidence suggests that ID in early pregnancy can negatively affect fetal neurodevelopment, resulting in lasting cognitive and psychological disorders.
Anemia, Affecting Millions in the US, Varies in Treatment

Anemia is a prevalent blood disorder affecting millions of Americans. It is characterized by insufficient red blood cells or dysfunctional ones, and this leads to low hemoglobin levels and a variety of symptoms like weakness, dizziness, and fatigue. Several conditions can increase the risk of developing anemia, including chronic diseases like kidney disease, cancer, and autoimmune disorders, as well as life stages such as pregnancy. It’s essential to recognize the symptoms early, as many people don’t realize they have anemia until it’s diagnosed through a blood test.
Iron Deficiency and Anemia: A Cycle of Nutritional Deficiency Impacting Women Globally

Iron deficiency (ID) is the most prevalent nutritional deficiency worldwide, significantly affecting women due to increased iron demands during pregnancy and menstruation. This condition often progresses to iron deficiency anemia (IDA), characterized by severe fatigue and cognitive impairments. IDA disproportionately impacts low-income groups who lack access to nutritious food and healthcare.
Iron Deficiency Anemia Impacts 25% Worldwide

Anemia, particularly iron deficiency anemia (IDA), affects nearly a quarter of the global population, driven predominantly by iron deficiency. This condition disproportionately impacts preschool children, pregnant and non-pregnant women, as well as individuals with chronic conditions such as kidney disease, cancer, or those undergoing certain surgeries. Iron homeostasis, critical to managing IDA, relies primarily on regulated absorption rather than excretion, with the peptide hormone hepcidin playing a crucial role by modulating iron uptake based on the body’s needs.
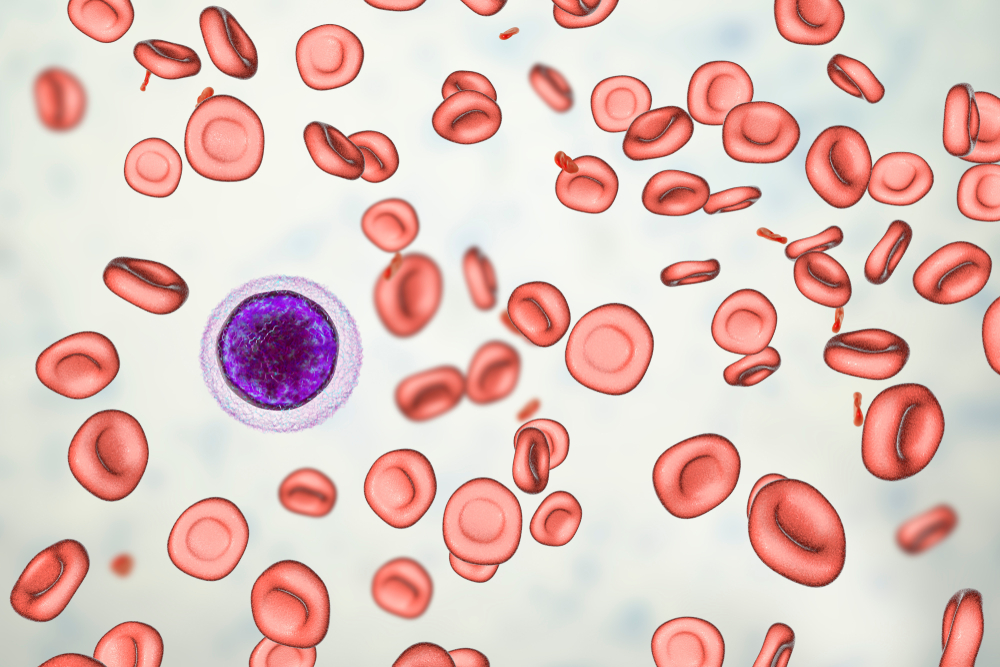
Iron-Deficiency Anemia: Understanding Risks, Prevention, and Treatment

Iron-deficiency anemia, the most prevalent type of anemia, arises when the body lacks sufficient iron to produce healthy red blood cells. Symptoms may not appear in mild cases but can include fatigue, dizziness, and chest pain as the condition worsens. Causes of this deficiency range from blood loss due to gastrointestinal issues or menstruation, to poor iron absorption from various health conditions and surgeries. Furthermore, certain chronic diseases and lifestyle choices, like endurance sports, can exacerbate the problem by impairing iron absorption or increasing iron loss.
Study Shows IV Iron Outperforms Oral Iron for Anemia in Gujarati Pregnant Women

In a prospective cost-effectiveness study conducted in Gujarat, India, 188 pregnant women with moderate to severe anemia were compared based on the type of iron treatment received—either intravenous iron sucrose (IVIS) or oral iron (OI). The participants, enrolled during their 14 to 18 weeks of pregnancy from two districts, were tracked through their pregnancy up to the postpartum phase at 42 days. The study measured the changes in hemoglobin levels at various stages, with the IVIS group showing a significant increase from an initial average of 8.2 g/dl to 11.45 g/dl, while the OI group experienced a decrease from 9.99 g/dl to 9.55 g/dl.
Advancements in Postpartum Anemia Care Reveal Global Healthcare Gaps
Recent advancements have been made in the early detection and treatment of postpartum anemia (PPA), a condition that severely impacts mothers’ physical and mental health. However, a gap remains in widespread implementation, partly due to a lack of awareness among healthcare providers about the latest research and effective treatment protocols. This includes iron supplementation, which has shown significant benefits in improving women’s postpartum wellbeing.
Anemia in Pregnancy: A Public Health Challenge Requiring Enhanced Interventions
Anemia during pregnancy, particularly iron deficiency anemia (IDA), poses a significant health challenge, with a prevalence rate varying between 6.9% and 28.7% in the United States, influenced by racial, ethnic, and socioeconomic factors. Data from the WIC program indicate that about 10% of participating pregnant women suffer from anemia, classified as a mild to moderate public health risk, especially among Black women and those diagnosed in later pregnancy stages. This situation calls for enhanced public health interventions and strategies.
Women’s Health: The Impact of Iron Deficiency

A narrative review discussed current definitions, causes, and treatment of iron deficiency and anaemia in women. Researchers noted that current treatments fall short, needing advancements in safer, more effective iron supplements and more data on intravenous iron. The narrative concluded that collaboration with patients and public is vital for effective research, particularly in new iron dosing methods and evaluating intravenous iron’s long-term role.